During my practice as a perioperative nurse, an increase in specimen mishandling and near-misses were observed. The data in our unit showed a remarkable trend which is a 600% increase in patient safety incidents related to specimen irregularities within the operating room. To us, this represents a substantial increase since our error threshold to this issue is zero. According to Association of Peiroperative Nurses (2019), there is no margin of error for specimens since it can harm the patient due to delayed and incorrect diagnosis. These incidents occurred within a sample size of 2,697 specimens processed by the main operating room between the months of April to November 2022, resulting in a probability of 2 errors in every 1,000 specimens sent. These findings are a cause for serious concern due to the potential consequences of specimen irregularities or errors which include adverse patient outcomes or misdiagnosis, grievances, legal proceedings, and substantial financial losses. I have used the Plan Do Study Act (PDSA) methodology in order to identify the root causes of the specimen errors and brainstorm possible solutions to address the causes of specimen errors. It was found out that ineffective communication, delays in patient transport, poor documentation, and short turnaround time between each case were the main causes of such errors and near-misses. My interventions were based on the similar quality improvement study in the Joint Commission Journal (2021) wherein they were able to reduce their errors from 10:1,000 down to 2.31:1000 through multidisciplinary interventions focusing on enhanced communication, standardized specimen reconciliation process, and the use of specimen request form. (Holstine & Samora, 2021)
In my PDSA study, I have identified 16 True Root Causes which contributed to near misses and specimen errors within our unit as shown in the table I have made before.
While it is important for us to implement all the identified possible solutions in order to address the true root causes, prioritization of solutions using effort-impact diagram and prioritization matrix was used. Out of the 12 identified solutions for the cluster of root causes, we have identified 9 priority interventions with low-cost and low-effort that will yield the most desirable result in maintaining our zero threshold in specimen processing. These include the development of specimen manuals, early hand off of bedside to perioperative nurses, monitoring of expected specimen numbers, enhanced reporting mechanisms, establishment of a channel for swift issue resolution, integration of specimen endorsements to schedule confirmation, and a two-way validation system postoperatively. Below was my prioritization matrix I used.
Our intervention phase started in December of 2022 which drastically decreased the error incidence until February 2024. Why until February 2024 only? Because that was the month I transferred from OR to the ICU, and I have no idea of the figures as of the present.
Through these interventions with low cost from our institution, we were able to maintain below our threshold for specimen error. I would say that it is really fun and at the same time fulfilling having a quality improvement project in healthcare since we know that patient safety is at stake. If I will face the same situation again, with enough time and cooperation from the unit, I would love to start another quality improvement project. As a matter of fact, I have a quality improvement project ongoing right now but I wasn’t able to finish it yet due to time constraints. It is always in my mind not to blame someone alone for errors resulting in patient harm. As nurses, we should always see these patient-safety related incidences as an opportunity to investigate the current system that we have. While my previous PDSA leans toward enhancement of the past specimen protocol that we have, I am now doing project improvements in manpower training. While flawed systems can undoubtedly result in patient safety incidents, poor training can also be one of the true root-causes. Through enhanced training of medical staffs, the risk for patient harm decreases.
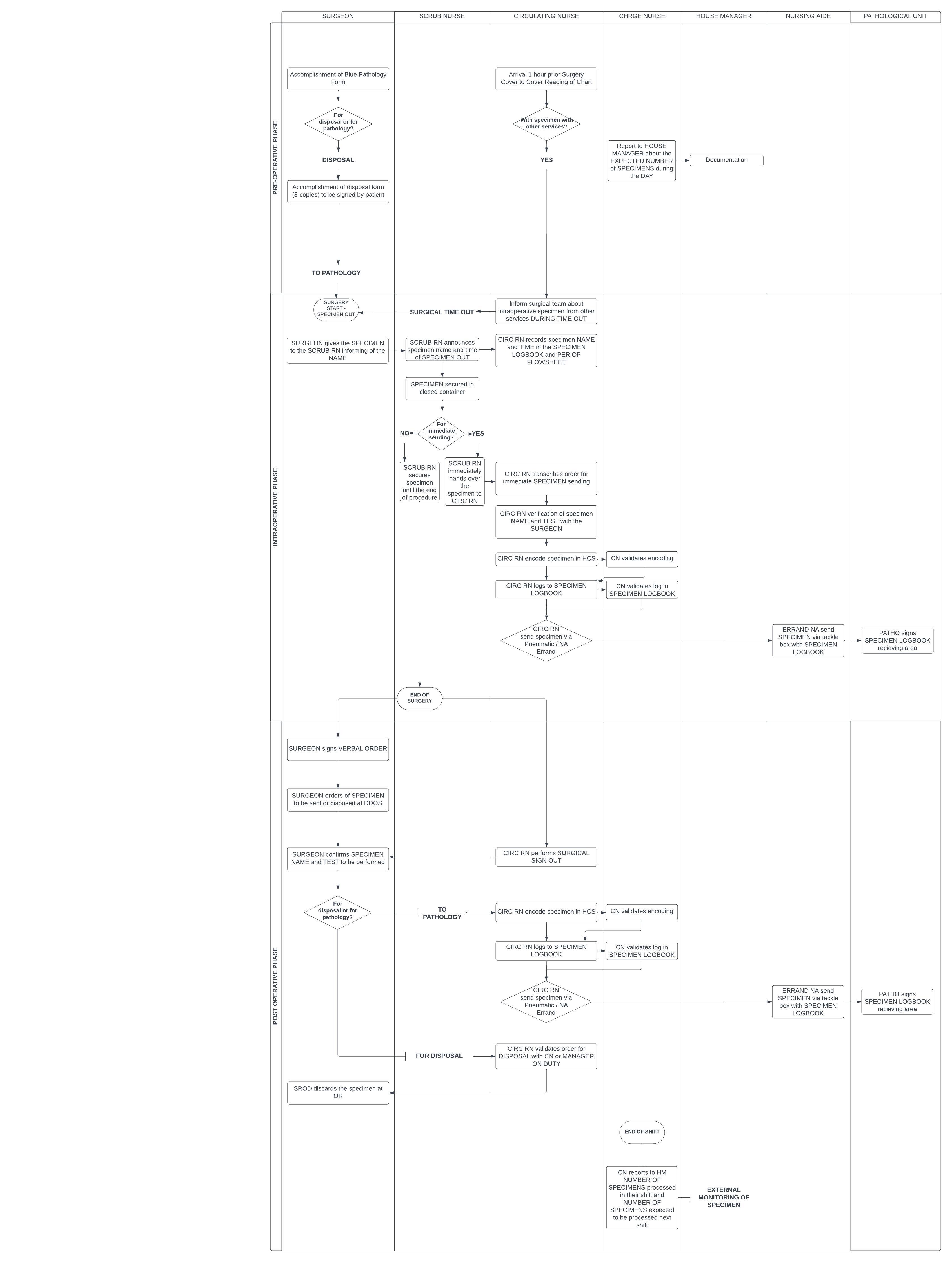
If you are interested of the improved protocol implemented, here is a swim lane to discuss the process. Please let me know if you have any questions!
Reducing Specimen Errors. (2019). AORN Journal, 109(4), 496–499. https://doi.org/10.1002/aorn.12658
Holstine, J. B., & Samora, J. B. (2021). Reducing Surgical Specimen Errors Through Multidisciplinary Quality Improvement. The Joint Commission Journal on Quality and Patient Safety, 47(9), 563–571. https://doi.org/10.1016/j.jcjq.2021.04.003